Share this post:
Author: Kristin Watson, PharmD, BCPS-AQ Cardiology
It is well documented that peripheral arterial disease (PAD) is associated with an increased risk of myocardial infarction and stroke, and it can significantly impact quality of life. Unfortunately, detection and treatment rates are below optimal.1, 2 With 12% of those aged 40 years of age or older affected, how do clinicians decide who and when to screen given their limited time with patients?1
It is a common misconception that many patients with PAD have “classic” symptoms, such as lower extremity pain or cramps that occur with exertion and are relieved with rest. This belief can lead to falsely low rates of diagnosis and treatment. Classic symptoms occur in only 1 of 10 patients and nearly half have no symptoms at all. Remaining patients will have a variety of atypical symptoms.1, 3 Additionally, symptoms may be masked or exertional capability may be hindered by other disorders such as heart failure, osteoarthritis, and spinal stenosis.
Since a limited number of patients have symptoms, providers should assess for other signs of the disease and consider screening options for “asymptomatic” patients. Waiting for a complication to occur is not an acceptable option!
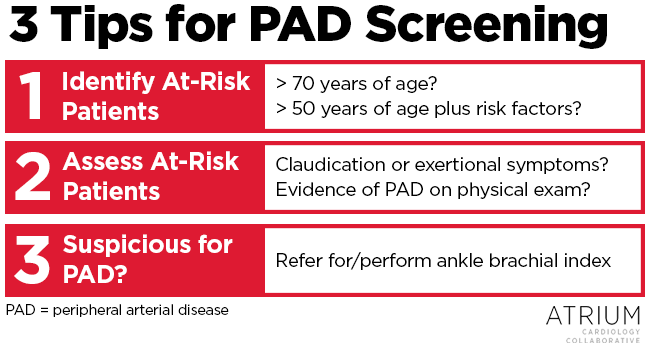
Here are some quick tips for determining who to screen in your own practice (Summarized in Figure 1).
- Identify the “at-risk population”
Older patients (> 70 years) and those over 50 years of age with additional risk factors, such as diabetes, hypertension, and smoking are at the highest risk for developing PAD.
- Ask patients about functional limitations
For example, what limits their walking distance? If pain develops during exertion, what relieves the pain? If the patient is not physically active, find out why… maybe lower extremity pain is preventing them from getting up and moving!Check out these validated instruments for assessing claudication symptoms and determine which would fit best in your practice: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2560464/ and http://www.ncbi.nlm.nih.gov/pubmed/9546918
- Examine the lower extremities
Is there hair loss? Are the dorsalis pedis and posterior tibial pulses present or are these diminished? What is the temperature and color? Are non-healing wounds present? Physical examination is one of our best tools for detecting PAD! And it is free too!
- Refer for further evaluation
If symptoms or physical exam findings are suspicious for PAD, the patient should be referred for further screening to confirm the diagnosis. The ankle to brachial index (ABI) is a relatively simple test that can completed in the clinic using a hand-held Doppler, although it often requires additional personnel, time, and resources.
There is ongoing debate regarding the utility of ABI screening in asymptomatic, high-risk patients, as these individuals are already candidates for aggressive risk factor reduction (e.g., smoking cessation, statin therapy, and blood pressure control), which is the cornerstone of PAD treatment. Evidence supporting the use of ABI screening to improve outcomes in this population is still lacking. However, the counterargument is that this group should be referred for ABI testing early to ensure that risk-reduction therapies are adequate.
A summary of national guideline recommendations can be found in the table below.
| Organization | Who to Screen | How to Screen |
| American College of Cardiology Foundation/American Heart Association (2011)4 | 50 years of age or older AND risk factors for atherosclerosisOR 70 years of age or older | At risk patients:
ABI test if PAD suspected (one or more of the following):
|
| American Diabetes Association (2016) 5,6 | All patient with diabetes | Assess for presence of symptoms and pedal pulses.ABI test if:
|
| U.S. Preventative Services Task Force (2013)7 | For adults without PAD, cardiovascular disease, severe chronic kidney disease or diabetes: insufficient data to determine the risk vs. benefit of ABI screening for PAD. | N/A |
Stayed tuned for future features on physical assessment skills that you can integrate into your own practice!
 |
Kristin Watson, PharmD, BCPS-AQ Cardiology
|
References
- Mozaffarian D, Benjamin EJ, Go AS, et al . AHA statistical update: heart disease and stroke statistics – a report from the American Heart Association. Circulation 2016;133:e38-360.
- Hirsch AT, Criqui MG, Treat-Jacobson D, et al. Peripheral arterial disease detection, awareness and treatment in primary care. JAMA 2001;286:1317-24.
- McDermott MM, Greenland P, Liu K, et al. Leg symptoms in peripheral disease: associated clinical characteristics and functional impairment. JAMA 2001;286:1599-1606.
- Anderson JL, Halperin JL, Albert N, et al. Management of patients with peripheral artery disease (compilation of 2005 and 2011 ACCF/AHA guideline recommendations): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2013;61:1555-70.
- American Diabetes Association. Peripheral arterial disease in people with diabetes. Diabetes Care 2003;26:3333–41.
- American Diabetes Association. Microvascular complications and foot care. Diabetes Care. 2016;39:S72-80.
- Moyer VA, on behalf of the U.S. Preventive Services Task Force. Screening for peripheral artery disease and cardiovascular disease risk assessment with the ankle–brachial index in adults: U.S. preventive services task force recommendation statement. Ann Intern Med 2013:159:342-8.
Share this post: