Share this post:
Author: Stormi Gale, PharmD, BCPS
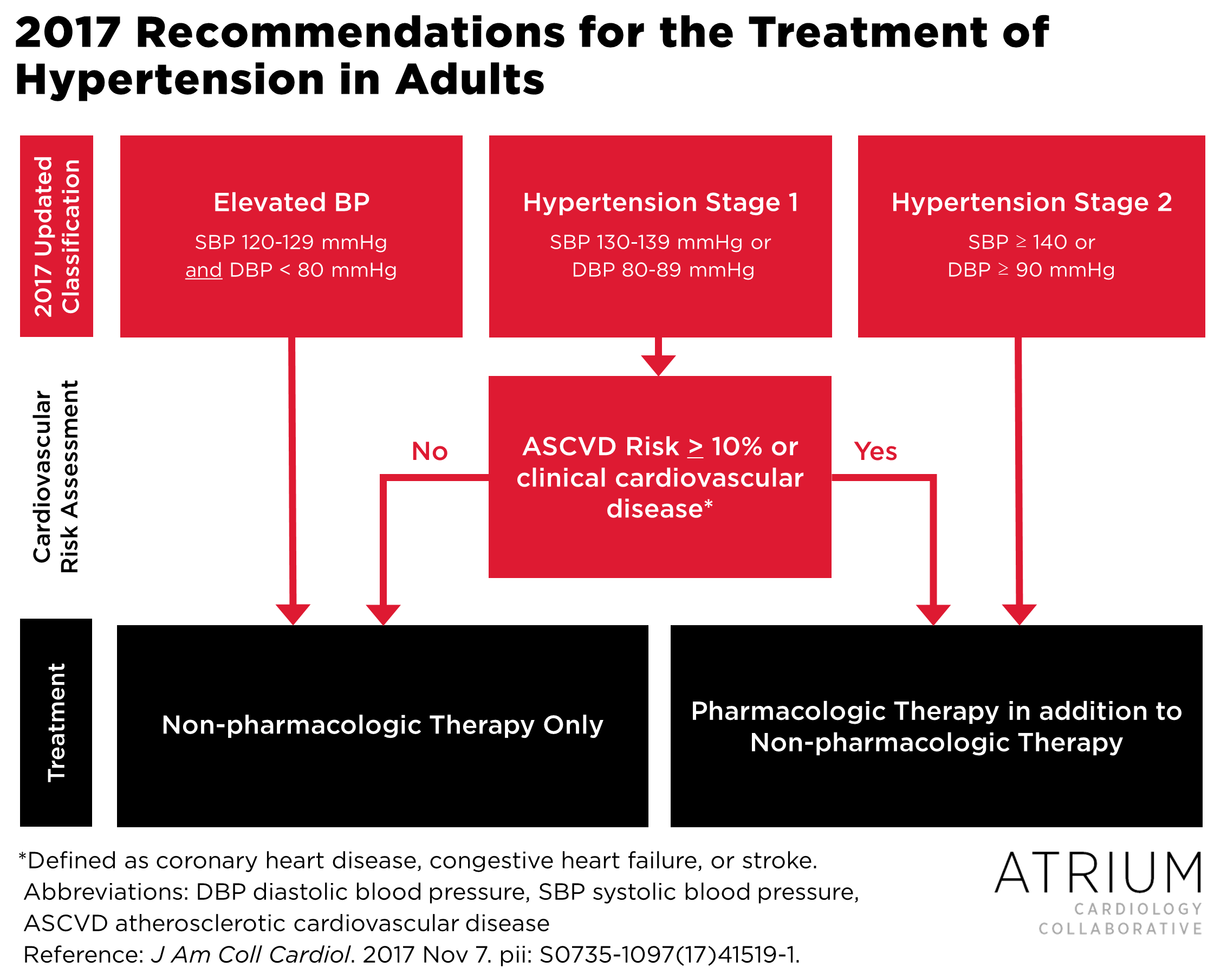
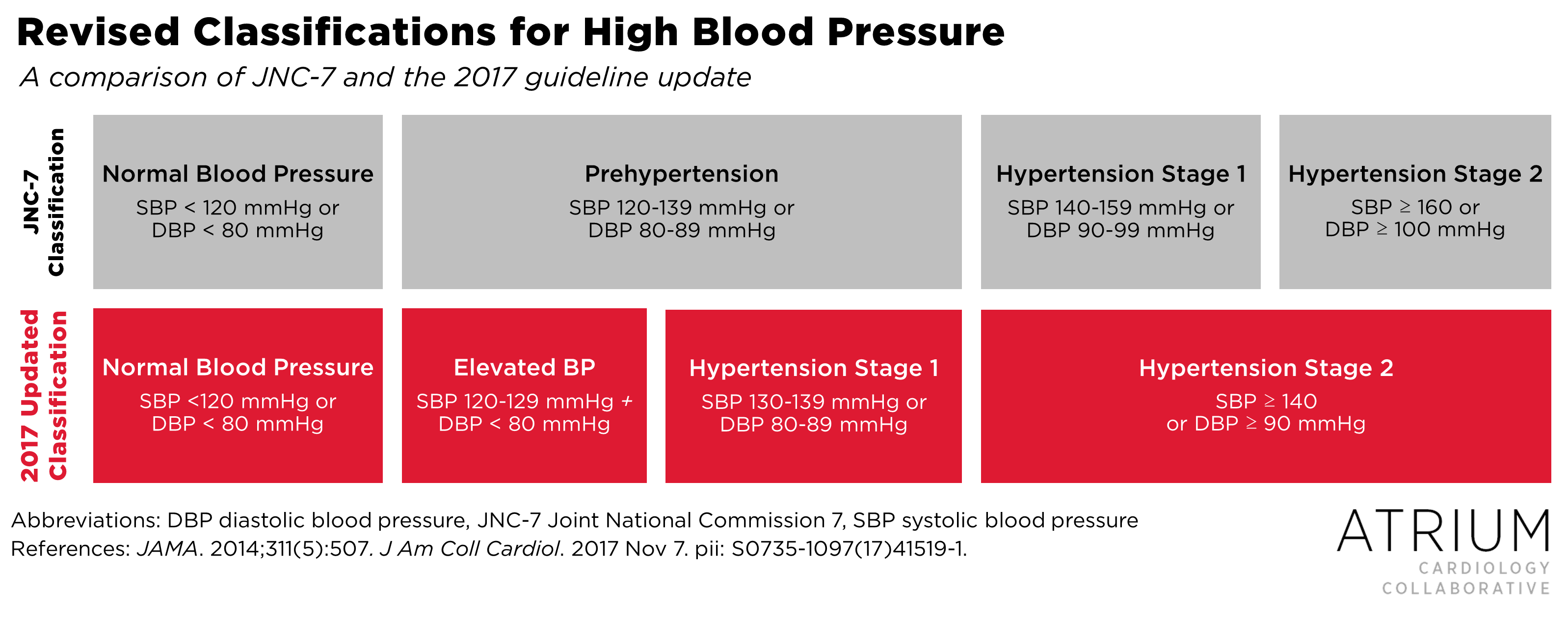
One of the major changes in the new guidelines is revised staging definitions, which includes removal of the term Prehypertension, the addition of an Elevated Blood Pressure group, and more stringent criteria for both Stage 1 and Stage 2 hypertension (see Figure 1 for a comparison of changes between JNC-8 and the 2017 guidelines).1,2 Much of the buzz surrounding the new guidelines has centered around the fact that almost half of Americans now meet criteria for hypertension according to the new staging definitions.1 Despite an increase in the number of patients who meet diagnostic criteria for hypertension (from 31.9% to 45.6% since the publication of JNC-7 in 2004), the percentage of patients who will require pharmacologic therapy has only increased from 34.3% to 36.2% within the same time frame.3 This disproportionate change is largely attributable to the expanded role of atherosclerotic cardiovascular disease (ASCVD) risk scoring, which has now been integrated as a key decision point in the hypertension management algorithm (see Figure 2).1 For those without preexisting ASCVD, initiation of pharmacologic therapy for Stage 1 hypertension is dependent on 10-year ASCVD risk, i.e., patients with < 10% risk only require lifestyle modifications whereas those with > 10% risk should be initiated on pharmacologic therapy in addition to lifestyle modifications.
Figure 1
 Another major change in the new guidelines is the threshold for Stage 1 vs Stage 2 hypertension (Figure 2). Under the old guidelines, patients with Stage 2 hypertension required initiation of two antihypertensive medications. However, under the new guidelines the recommendation for management of Stage 2 hypertension suggests initiating two agents only if the patient’s blood pressure is 20/10 mmHg above goal, or for systolic blood pressure (SBP) > 150 mmHg. These new recommendations are only slightly more rigorous than what was recommended in JNC-8.2
Another major change in the new guidelines is the threshold for Stage 1 vs Stage 2 hypertension (Figure 2). Under the old guidelines, patients with Stage 2 hypertension required initiation of two antihypertensive medications. However, under the new guidelines the recommendation for management of Stage 2 hypertension suggests initiating two agents only if the patient’s blood pressure is 20/10 mmHg above goal, or for systolic blood pressure (SBP) > 150 mmHg. These new recommendations are only slightly more rigorous than what was recommended in JNC-8.2
Most of the evidence for the 2017 goals are derived from the Systolic Blood Pressure Intervention Trial (SPRINT) trial, which was covered in a previous post here.4 In summary, SPRINT compared an intensive SBP target (< 120 mmHg) to a less stringent target (< 140 mmHg) in 2,636 patients of at least 50 years of age who were at an increased risk of cardiovascular events. The trial was terminated early due to overwhelming benefits in the intensive therapy group, including a reduction in the primary composite outcome of myocardial infarction, other acute coronary syndromes, stroke, acute decompensated heart failure, or death from cardiovascular causes, as well as a reduction in the individual endpoints of heart failure and all-cause death. The mean SBP achieved in the intensive-control group was 121.5 mmHg. Although stricter goals in the new guidelines seems like a drastic change, the adoption of < 130 mmHg is actually less aggressive than was studied in SPRINT.
Evidence that patients at low risk for cardiovascular events will benefit from strict antihypertensive management remains sparse, considering that these patients were excluded from SPRINT.4,5 The Heart Outcomes Prevention Evaluation (HOPE)–3 trial evaluated blood pressure lowering with fixed-dose combination antihypertensives in patients at intermediate risk for cardiovascular disease and found no difference in the coprimary composite outcomes of CV death, nonfatal MI, or nonfatal stroke with or without the addition of resuscitated cardiac arrest, heart failure, and revascularization.6 However, both of these composite outcomes were reduced with antihypertensive treatment in the subgroup of patients with a baseline SBP > 143.5 mmHg, supporting the recommendation to initiate pharmacologic therapy in all patients with Stage 2 hypertension and reserving it to Stage 1 patients who also have an increased risk for ASCVD.
In terms of patient subgroups, the implications of the updated guidelines are probably greatest for older patients. Historically, more lenient goals have been recommended in older patients as a means of avoiding adverse effects.2 However, the updated SBP goal of 130 mmHg also applies to patients 65 years of age and older, with the exception of those who are institutionalized, no longer ambulatory, or have significant comorbidities that limit life expectancy (in whom more lenient targets could arguably be recommended regardless of age).1 No specific diastolic blood pressure (DBP) target is recommended in older patients, as isolated SBP has been shown to be the principal form of hypertension in patients above 65 years of age, and cardiovascular benefits have been observed with lowered SBP regardless of differences in DBP.7–12 A sub-analysis of patients > 75 years-old in SPRINT provides further evidence for these changes.13 Stringent blood pressure control (< 120 mmHg) showed an even greater cardiovascular benefit in the older patient subgroup than what was demonstrated in the overall population. Furthermore, despite the concern for adverse effects in older patients (particularly orthostasis and falls), no differences in serious side effects were observed between intensive and standard treatment. Unexpectedly, a trend toward a lower risk of orthostatic hypotension with dizziness and injurious falls was observed in the intensive therapy group, although this was not statistically significant.
Despite an expanding number of eligible patients, treatment recommendations are generally similar to those made in JNC-8.1,2 The new guidelines continue to emphasize non-pharmacologic therapies, including increased physical activity and a diet limited in sodium, alcohol, saturated fat, and total fat, but increased potassium supplementation. In terms of pharmacologic therapy, thiazide-type diuretics, calcium channel blockers, angiotensin-converting enzyme (ACE) inhibitors, and angiotensin II receptor blockers (ARBs) remain first-line (to be chosen based on patient-specific factors and comorbid indications), and spironolactone continues to be preferred in patients with resistant hypertension or a diagnosis of primary hyperaldosteronism.
Although recommendations for drug selection remain relatively unchanged, one of the most exciting updates for pharmacists is the emphasis on multidisciplinary team-based care in the treatment of this growing patient population.1 The guidelines recognize the surmounting evidence suggesting that the addition of nurse and/or pharmacist-driven intervention improves blood pressure control compared to usual care.14–18 Although many health-systems and ambulatory care clinics have already embraced opportunities to expand pharmacists’ contributions, expect further integration of multidisciplinary team members into patient care models in the future.
In summary, the updated guidelines do not significantly change what we use to treat, but in whom we treat and to what end (see Table 1 for details). The use of ASCVD risk calculations will determine initiation of pharmacologic therapy in patients without preexisting disease, and goals in older patients no longer differ from younger populations. Emphasized strategies for improved BP control include team-based care and out-of-office BP monitoring.
So, if your New Year’s resolutions include keeping up with the latest trends, remember that prehypertension is a thing of the past, and 130 is the new 140.
| Table 1. Summary of Major Changes in the 2017 High Blood Pressure Guidelines |
|
 |
Stormi Gale, PharmD, BCPS
|
References:
- 2017 Hypertension Clinical Practice Guidelines | Hypertension.
- James PA, Oparil S, Carter BL, et al. 2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults: Report From the Panel Members Appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507.
- Muntner P, Carey RM, Gidding S, et al. Potential U.S. Population Impact of the 2017 American College of Cardiology/American Heart Association High Blood Pressure Guideline. Circulation. November 2017:CIRCULATIONAHA.117.032582.
- The SPRINT Research Group. A Randomized Trial of Intensive versus Standard Blood-Pressure Control. N Engl J Med. 2015;373(22):2103-2116.
- Optimal systolic blood pressure target, time to intensification, and time to follow-up in treatment of hypertension: population based retrospective cohort study | The BMJ.
- Lonn EM, Bosch J, López-Jaramillo P, et al. Blood-Pressure Lowering in Intermediate-Risk Persons without Cardiovascular Disease. N Engl J Med. 2016;374(21):2009-2020.
- Egan BM, Li J, Hutchison FN, Ferdinand KC. Hypertension in the United States, 1999 to 2012: progress toward Healthy People 2020 goals. Circulation. 2014;130(19):1692-1699.
- Liu X, Rodriguez CJ, Wang K. Prevalence and trends of isolated systolic hypertension among untreated adults in the United States. J Am Soc Hypertens JASH. 2015;9(3):197-205.
- Staessen JA, Fagard R, Thijs L, et al. Randomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension. The Systolic Hypertension in Europe (Syst-Eur) Trial Investigators. Lancet Lond Engl. 1997;350(9080):757-764.
- Liu L, Wang JG, Gong L, Liu G, Staessen JA. Comparison of active treatment and placebo in older Chinese patients with isolated systolic hypertension. Systolic Hypertension in China (Syst-China) Collaborative Group. J Hypertens. 1998;16(12 Pt 1):1823-1829.
- Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program (SHEP). SHEP Cooperative Research Group. JAMA. 1991;265:3255-64. – Google Search.
- Beckett NS, Peters R, Fletcher AE, et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008;358(18):1887–1898.
- Williamson JD, Supiano MA, Applegate WB, et al. Intensive vs Standard Blood Pressure Control and Cardiovascular Disease Outcomes in Adults Aged ≥75 Years: A Randomized Clinical Trial. JAMA. 2016;315(24):2673-2682.
- Carter BL, Rogers M, Daly J, Zheng S, James PA. The potency of team-based care interventions for hypertension: a meta-analysis. Arch Intern Med. 2009;169(19):1748-1755.
- Clark CE, Smith LFP, Taylor RS, Campbell JL. Nurse led interventions to improve control of blood pressure in people with hypertension: systematic review and meta-analysis. BMJ. 2010;341:c3995.
- Santschi V, Chiolero A, Colosimo AL, et al. Improving blood pressure control through pharmacist interventions: a meta-analysis of randomized controlled trials. J Am Heart Assoc. 2014;3(2):e000718.
- Carter BL, Coffey CS, Ardery G, et al. A Cluster-randomized Trial of a Physician\Pharmacist Collaborative Model to Improve Blood Pressure Control. Circ Cardiovasc Qual Outcomes. 2015;8(3):235-243.
- Tsuyuki RT, Al Hamarneh YN, Jones CA, Hemmelgarn BR. The Effectiveness of Pharmacist Interventions on Cardiovascular Risk: The Multicenter Randomized Controlled RxEACH Trial. J Am Coll Cardiol. 2016;67(24):2846-2854.
Share this post: