Share this post:
Author: Kristin Watson, PharmD, BCCP
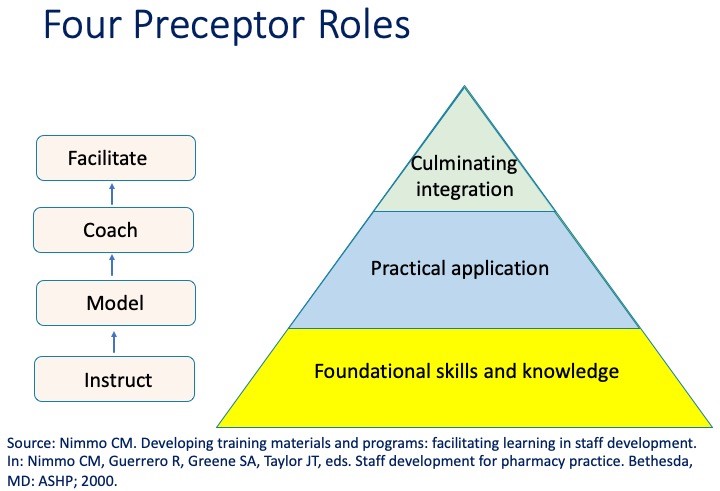
In part one of this blog, the preceptor roles – instruct and model – were discussed. The remaining preceptor roles – coach and facilitate – will be discussed in this post. Applying these roles provides a framework to enable our learners to transition from learning core concepts towards becoming independent, clinical-problem solvers (Figure). You may find that a learner may be reluctant to transition to one of these roles. It is important to be encouraging and to let the learner know that they are able to progress because you are confident in their abilities.
Coach
It is now time for the learner to put their skills to work. Foundational skills have be laid for the learner through prior education, training or by the preceptor. Before handing over the reins, preceptors should observe their learners performing tasks/skills expected to occur during the learning experience. When the coaching phase is reached, preceptors should observe the learner and provide feedback. The preceptor should have learners “think out loud”, when possible, and let the preceptor in on his/her thought process.
It may not always be feasible/realistic to have the learner tell you what he/she is thinking in a given situation. For example, a student is going to provide discharge counseling to a patient who was started on an oral anticoagulant: the preceptor can serve as a mock patient and identify any areas for improvement. A resident is going to give a recommendation on rounds regarding a change in therapy: the preceptor can first have the resident share his/her thoughts on why they plan to recommend a change in therapy. This helps ensure that the resident has the necessary data to support their recommendation. The preceptor can consider “challenging” the learner on the recommendation to help prepare the resident if the recommendation is not readily accepted. The preceptor can then observe the learner and provide feedback.
Additionally, it may not be feasible the preceptor to give direct feedback during the situation (e.g., learner conducting a patient interview). However, the preceptor should give the feedback as quickly as possible and be specific with their suggestions. Preceptors may find it necessary to “jump in” at times during a particular interaction. If so, it is important to avoid portraying the learner as ineffective. For example, the preceptor and learner can tell a patient that they are going to tag-team an interview. The learner will be the lead and the preceptor may ask follow-up questions. This approach sets the expectations for the interaction and can potentially eliminate the learner from feeling under-minded. Let the learner know up front that you encourage them to pay attention when you interject and that you will only do so when you feel when necessary. Be sure to debrief after this interaction so that the learner understands why you jumped in.
Preceptors should develop a checklist or a guide to determine when a learner is competent in a given role before giving independence. Preceptors should make it clear to learners that that he/she may not be able to be completely independent on the rotation, depending on their level of training/experience and progress. The expectations for independence should be outlined in the learning description and will likely differ for students, postgraduate year-1 and 2 residents.
Facilitate
It is now time for the learner to become independent with a particular task (e.g., participating in rounds, interviewing patients, etc.). Preceptors continue to be available during to answer questions and serve as a sounding board should challenging scenarios arise. Additionally, preceptors should continue to review patients and facilitate topic discussions or journal articles with the learner. Learners should continue to be challenged even when the preceptor assumes the facilitation role. It is important to ensure that the learner’s skills and abilities continue to be molded.
Preceptors can consider “spot checking” the learner even after independence is gained. This enables the processes of on-going feedback. Additionally, it provides the preceptor the opportunity to determine if there are areas in which the preceptor needs to employ earlier preceptor roles. Transparency about this process is important so as not to affect the learner’s confidence if one shows up announced to observe them “in action”.
Learners should be encouraged to reflect on their own performance when performing tasks independently. Preceptors will likely need to guide learners on this process. Suggest giving examples of how one conducts their own self-evaluation and provide examples of what self-evaluation strategies has worked well for other learners. Preceptors should take time to seek the learner’s evaluation of their own performance; probing questions may be needed to stimulate this conversation. This step is critical as learners may identify areas that they perceive to be challenges that were not recognized by the preceptor. The preceptor can then work with the learner to determine which steps, if any, need to be taken to assist the learner.
In summary, the four preceptor roles are an excellent guide to enable us to structure our rotation. The use of these roles should be paired with clear expectations and feedback. Tailoring the learning experience for each learner will afford them the opportunity to grow and may make the learning experience even more rewarding for the preceptors. Which roles to apply for a given learning experience should based on each trainee’s level of education and prior experience in conjunction with the goals and structure of your rotation.
 |
Kristin Watson, PharmD, BCCP
|
For more on this topic check out:
- American Society of Health-System Pharmacists. Starring Roles: The four preceptor roles and when to use them. Available: http://www.ashpmedia.org/softchalk/softchalk_preceptorroles/softchalk4preceptorroles_print.html
- Weitzel, KW, Walter EA, Taylor. Teaching clinical problem solving: a preceptor’s guide. Am J Health-Sys Pharm. 2012;69:1588-99.
Share this post: