Share this post:
Authors: Jeremy Pollock, MD and Stormi Gale, PharmD, BCCP
Questions regarding the role of sodium-glucose co-transporter-2 (SGLT2i) in heart failure with reduced ejection fraction (HFrEF) have been raised since the publications of EMPA-REG OUTCOME in 2015.1 Despite being designed to assess cardiovascular risks in patients with diabetes, empagliflozin was associated with reductions in heart failure (HF) hospitalizations. Subsequent results from CANVAS and DECLARE-TIMI 58 suggested the benefits in HF are likely a class effect, although these studies only included a small number of patients with pre-existing heart failure.2,3 The results of the Study to Evaluate the Effect of Dapagliflozin on the Incidence of Worsening Heart Failure or Cardiovascular Death in Patients With Chronic Heart Failure (DAPA-HF), presented at the 2019 European Society of Cardiology Congress, shed light on the potential for these medications in HFrEF.
Summary of DAPA-HF
DAPA-HF evaluated the effects of dapagliflozin in 4,744 patients with symptomatic HFrEF and an elevated N-terminal pro–B-type natriuretic peptide.4,5 Patients with eGFR < 30 ml/min/1.73 m2, symptomatic hypotension or systolic blood pressure < 95 mmHg, or type 1 diabetes mellitus were excluded. A diagnosis of type II diabetes was not required; overall, less than half of the patients enrolled had diabetes. The majority of patients enrolled had class II or III HF (68% and 32%, respectively) and a mean ejection fraction of 31%. About half of patients had ischemic cardiomyopathy.. The majority of patients were on appropriate guideline-directed medical therapy, with 94%, 96%, and 71% of patients enrolled on renin-angiotensin system inhibitors (RASi), beta-blockers (BB), and mineralocorticoid receptor antagonists (MRA), respectively.
After a mean follow-up of 18.2 months, dapagliflozin reduced the primary outcome of cardiovascular death, hospitalization for HF, or urgent HF visit compared to placebo (HR 0.74, 95% CI 0.65-0.85; p=0.00001), with a number needed to treat of 21. In addition to benefits in all three of the individual components of the composite primary endpoint, dapagliflozin also reduced the relative risk of all-cause mortality by 17% (HR 0.83, 95% CI, 0.71-0.97; p=0.022). Importantly, the benefits of dapagliflozin were consistent in patients both with and without a diagnosis of diabetes.
So what does this mean for current practice?
Many cardiologists have shied away from these agents due to unfamiliarity and perceived safety concerns (ie, genital infections, diabetic ketoacidosis). It’s worth noting that in clinical trials many of the commonly cited adverse effects were similar to placebo (although it may be reasonable to avoid canagliflozin due to the increased risk of lower limb amputations).2 Furthermore, it is expected that updated guidelines will include SGLT2i as a treatment option in HF.
The optimal time to initiate SGLT2 inhibitors remains unanswered. Currently, SGLT-2 inhibitors should be considered for all patients with HFrEF (on GDMT) and adequate renal function (i.e., CrCl > 30 mL/min) who are not hypotensive. Additional studies are underway to evaluate the role for these agents in patients with advanced kidney disease, although this class has been shown to elicit renoprotective effects in other populations.3
Bottom Line
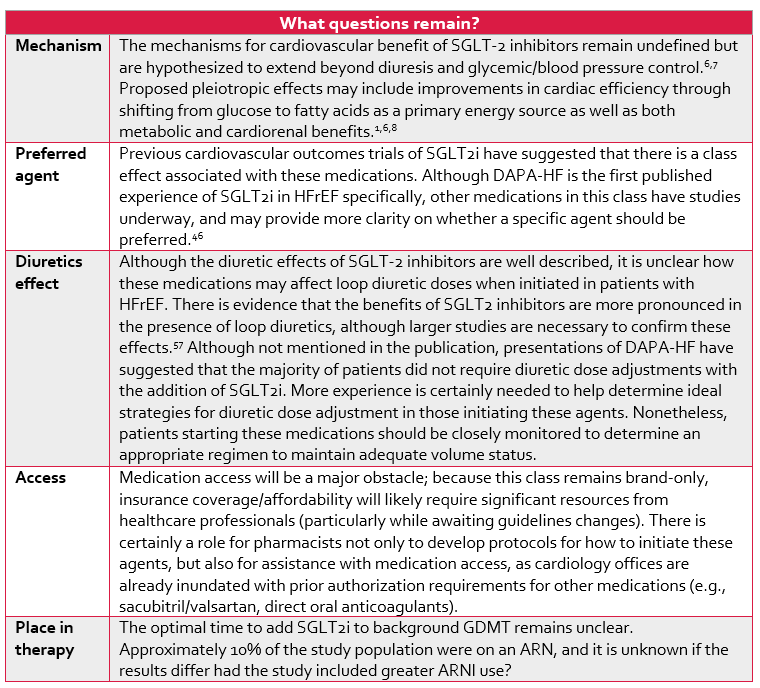
Despite the impressive outcomes demonstrated in DAPA-HF, SGLT2i prescribing has historically been limited to endocrinologists and primary care, and resistance amongst cardiologists remains. An interesting analogy was presented several times at the 2019 Heart Failure Society of America Annual Meeting. Statins used to be considered “endocrinology” drugs prior to published evidence of benefit in cardiovascular disease, and now are a standard of care within cardiology.6 As such, we urge cardiologists to embrace this class of therapy in a similar manner. DAPA-HF is perhaps the most practice-changing study in HFrEF since the publication of PARADIGM-HF in 2014. It is expect that these agents will be added as an option in the next HF guideline update, and should be considered in all patients with HFrEF on established GDMT. Before then, however, it will be prudent for cardiologists to gain familiarity with the prescribing and monitoring of these medications, as there is a clear benefit in patients with HFrEF despite adequate background therapy.
 |
Jeremy Pollock, MD
|
 |
Stormi Gale, PharmD, BCCP
|
References:
- Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes. N Engl J Med. 2015;373(22):2117-2128.
- McMurray JJV, DeMets DL, Inzucchi SE, et al. The Dapagliflozin And Prevention of Adverse-outcomes in Heart Failure (DAPA-HF) trial: baseline characteristics. Eur J Heart Fail. 0(0).
- McMurray JJV, Solomon SD, Inzucchi SE, et al. Dapagliflozin in Patients with Heart Failure and Reduced Ejection Fraction. N Engl J Med. September 2019:NEJMoa1911303.
- Neal B, Perkovic V, Mahaffey KW, et al. Canagliflozin and Cardiovascular and Renal Events in Type 2 Diabetes. N Engl J Med. 2017;377(7):644-657.
- Carbone S, Dixon DL. The CANVAS Program: implications of canagliflozin on reducing cardiovascular risk in patients with type 2 diabetes mellitus. Cardiovasc Diabetol. 2019;18(1):64.
- Gale SE, Poon JL, Watson K. Antihyperglycemic Medications and Impact on Cardiovascular Outcomes: A Review of Current Evidence. Pharmacother J Hum Pharmacol Drug Ther. 2018;38(7):739-757.
- Carbone S, Canada JM, Billingsley HE, et al. Effects of Empagliflozin on Cardiorespiratory Fitness and Significant Interaction of Loop Diuretics. Diabetes Obes Metab. 2018;20(8):2014-2018.
- EMPagliflozin outcomE tRial in Patients With chrOnic heaRt Failure With Reduced Ejection Fraction (EMPEROR-Reduced) – Full Text View – ClinicalTrials.gov.
Share this post: