Share this post:
Author: Stormi Gale, PharmD, BCCP
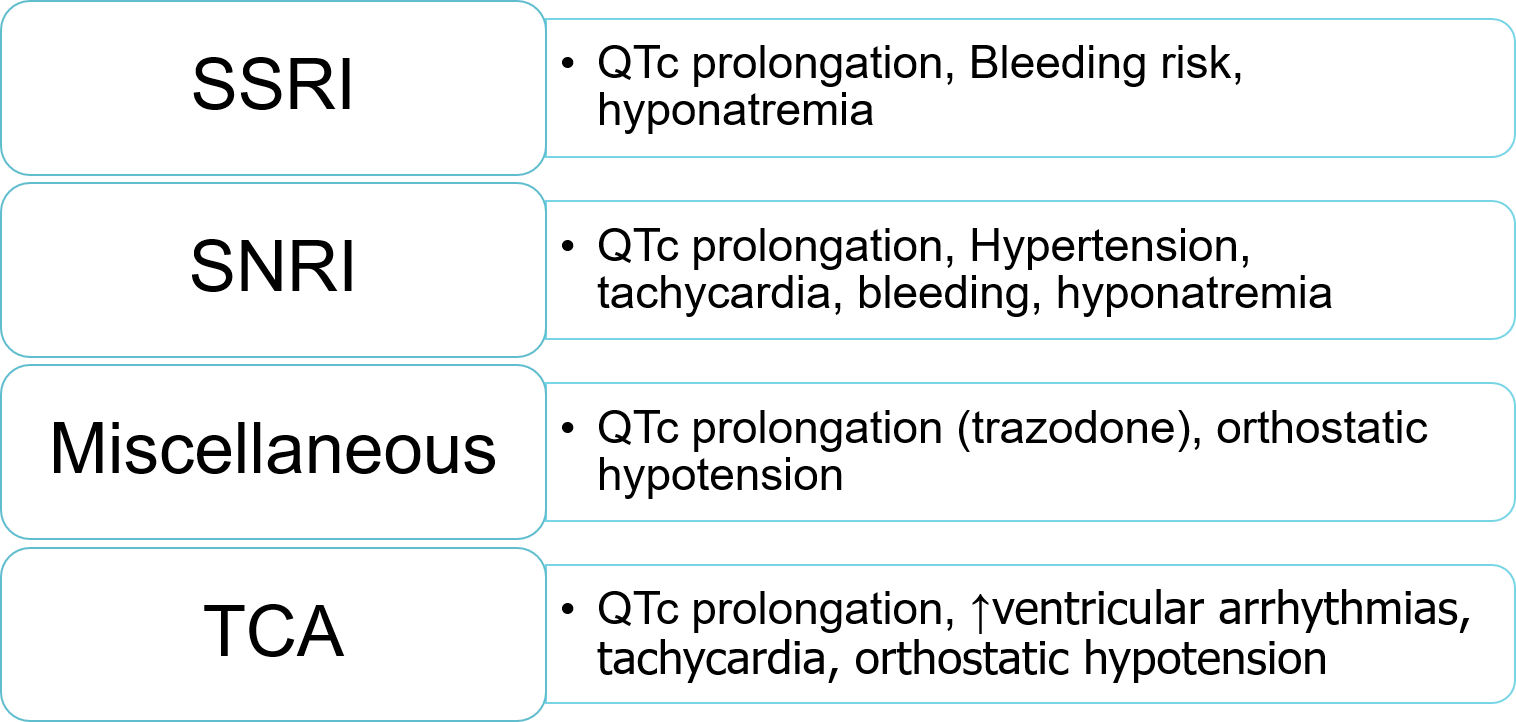
Depression is estimated to be as high as 40% in patients with heart failure (HF), with increasing prevalence as functional class worsens.1 Although depression is not commonly considered in the pathophysiology of heart failure, alterations in neurohormonal activation, including the sympathetic nervous system and inflammatory activity, can contribute to pathologic hemodynamic changes and remodeling. Depression is also associated with decreased adherence to cardioprotective medications and healthy lifestyle in other populations.2 Indeed, depression is considered to be an independent risk factor for CVD, and patients with HF and concomitant depression have been shown to have reduced survival and quality of life.3 Despite a poorer prognosis, few screening and management strategies have been shown to be effective in improving cardiovascular outcomes in patients with HF and concomitant depression.4 Nonetheless, national guidelines recommend screening of all patients with CVD and risk factors for depression; this can be done with the PHQ-2 and PHQ-9 questionaires.3 Additionally, safety of antidepressants in this population must be considered (Figure).
Figure 1: Safety of Antidepressants in Heart Failure
| SNRI, serotonin norepinephrine reuptake inhibitor; SSRI, selective serotonin reuptake inhibitor; TCA, tricyclic antidepressant |
A consensus regarding efficacy of treatment options is difficult to ascertain due to a high level of heterogeneity across various studies. The largest randomized, controlled trials to date have demonstrated pharmacological treatment with selective serotonin reuptake inhibitor (SSRIs) to be safe in patients with HF, but with mixed efficacy. In SADHART-CHF and MOOD-HF, there was no difference in depression or cardiovascular outcomes with placebo compared to sertraline and escitalopram, respectively.5,6 However, this is controversial as some data suggest an improvement in depression-related outcome with SSRI treatment.7 Nonetheless, SSRIs have consistently demonstrated safety in studies of patients with HF.5,6 The lack of benefit of depression treatment in patients with HF differs from data in coronary artery disease, in which SSRI therapy has been shown to improve outcomes.8
Comparably, recent nonpharmacologic data do not provide a clear direction on how to address depression in patients with HF. The Hopeful Heart trial found that using blended care with a psychiatrist, cardiologist, internist, and nurse improved health-related quality of life at 12 months compared to cardiovascular treatment alone in patients with systolic dysfunction who were recently hospitalized and scored positive for depression.9 However, there was no difference in readmission or mortality between groups.
Similarly, cognitive behavioral therapy may benefit depressive symptoms but has not been shown to improve heart failure outcomes.10 Perhaps the most promising data comes from the HF-ACTION trial, in which structured exercise programming improved depressive symptoms as well as hospitalization and mortality.11
Bottom Line
Depression is a common comorbidity in patients with heart failure that is associated with worse outcomes. Nonpharmacologic strategies such as cognitive behavioral therapy and structural exercise programs should be emphasized. Due to a lack of evidence for improved outcomes with pharmacologic therapies, the decision to use antidepressants should be patient-centered with preference for SSRIs given their proven safety in this population.
 |
Stormi Gale, PharmD, BCCP
|
Reviewed by: Sandeep Devabhakthuni, PharmD, BCCP
References
- Vaccarino V, Badimon L, Bremner JD, et al. Depression and coronary heart disease: 2018 ESC position paper of the working group of coronary pathophysiology and microcirculation developed under the auspices of the ESC Committee for Practice Guidelines. Eur Heart J.
- Gehi A, Haas D, Pipkin S, Whooley MA. Depression and Medication Adherence in Outpatients With Coronary Heart Disease: Findings From the Heart and Soul Study. Archives of Internal Medicine. 2005;165(21):2508-2513.
- Jha MK, Qamar A, Vaduganathan M, Charney DS, Murrough JW. Screening and Management of Depression in Patients With Cardiovascular Disease: JACC State-of-the-Art Review. J Am Coll Cardiol. 2019;73(14):1827-1845.
- Jünger J, Schellberg D, Müller-Tasch T, et al. Depression increasingly predicts mortality in the course of congestive heart failure. Eur J Heart Fail. 2005;7(2):261-267.
- O’Connor CM, Jiang W, Kuchibhatla M, et al. Safety and efficacy of sertraline for depression in patients with heart failure: results of the SADHART-CHF (Sertraline Against Depression and Heart Disease in Chronic Heart Failure) trial. J Am Coll Cardiol. 2010;56(9):692-699.
- Angermann CE, Gelbrich G, Störk S, et al. Effect of Escitalopram on All-Cause Mortality and Hospitalization in Patients With Heart Failure and Depression: The MOOD-HF Randomized Clinical Trial. JAMA. 2016;315(24):2683-2693.
- Gottlieb SS, Kop WJ, Thomas SA, et al. A double-blind placebo-controlled pilot study of controlled-release paroxetine on depression and quality of life in chronic heart failure. Am Heart J. 2007;153(5):868-873.
- Kim J-M, Stewart R, Lee Y-S, et al. Effect of Escitalopram vs Placebo Treatment for Depression on Long-term Cardiac Outcomes in Patients With Acute Coronary Syndrome: A Randomized Clinical Trial. JAMA. 2018;320(4):350-358.
- Belnap BH, Anderson A, Abebe KZ, et al. Blended Collaborative Care to Treat Heart Failure and Co-Morbid Depression: Rationale and Study Design of the Hopeful Heart Trial. Psychosom Med. 2019;81(6):495-505.
- Effects of Treating Depression and Low Perceived Social Support on Clinical Events After Myocardial Infarction: The Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) Randomized Trial. JAMA. 2003;289(23):3106-3116.
- Blumenthal JA, Babyak MA, O’Connor C, et al. Effects of exercise training on depressive symptoms in patients with chronic heart failure: the HF-ACTION randomized trial. JAMA. 2012;308(5):465-474.
Share this post: