Share this post:
Author: Stormi Gale, PharmD, BCPS
Case: EB is a 58-year-old African American man with ischemic cardiomyopathy (ejection fraction 35%) who presents to the emergency department for increasing dyspnea on exertion and bilateral extremity swelling. EB states that he just got back from a vacation and has not been following his usual low sodium diet (he gained 7 pounds while away), although he has been adherent to all medications. Upon exam, he appears to be in subset II (wet and warm) acute decompensated heart failure. His blood pressure is 114/76 mmHg and HR is 106 bpm. Your medication reconciliation reveals that EB takes the following heart failure medications at home: furosemide 60 mg daily, lisinopril 40 mg daily, carvedilol 25 mg twice daily, spironolactone 25 mg daily. All of his heart failure medications and doses have been stable for the past 6 months. EB is currently awaiting a bed on the cardiology unit.
Question: What would you do with his home carvedilol upon admission?
We’ve observed that beta-blockers are often discontinued in patients similar to EB. This is particularly bothersome in patients who have worked closely with their provider to slowly up-titrate their medications to at, or near, target doses over the course of months. As we’ll outline in this post, this common (but inappropriate) practice is largely a result of concerns related to the negative inotropic effects of beta-blockers and the fear that continuing them may worsen hemodynamics in the setting of all types of acute decompensated heart failure (ADHF).
While it may seem counterintuitive, beta-blockers should generally be continued during an episode of ADHF unless the patient has signs or symptoms of cardiogenic shock. In fact, discontinuing beta-blockers in the absence of shock can produce a deleterious rebound of sympathetic activity, including tachycardia, vasoconstriction, and increased fluid retention. These effects, coupled by renin-angiotensin-aldosterone activation, may paradoxicallyworsencardiac function during ADHF.1,2
As alluded to above, it’s also important to recognize that achieving goal doses – which have been shown to improve outcomes compared to lower doses – takes a significant amount of time and resources (for both patients and providers alike).3–5The “start low and go slow” approach is important for these medications, as the short-term negative inotropic effects of beta-blockers increase the risk of ADHF when titrated too quickly. Therefore, any time a beta-blocker is discontinued in a patient on a target dose, restarting at a low dose and slowly re-titrating (e.g., every 2 weeks) is required. Importantly, an exception to this rule would be patients in whom beta-blocker therapy was held for a minimal amount of time (e.g., only 24 hours), although a strict timeframe for this is not well-defined. For more information about dose titration, check out our recent YTV about optimizing beta-blocker therapy here.
Beta-blocker discontinuation in ADHF was evaluated in the Beta-blocker CONtinuation Vs. INterruption in patients with Congestive heart failure hospitalizED for a decompensation episode (B-CONVINCED) trial.6In this study, 169 patients with ADHF and a left ventricular ejection fraction of less than 40% who had been on a stable dose of a beta-blocker for at least 1 month were randomized to beta-blocker continuation versus discontinuation. Patients with contraindications to beta-blocker use, ST elevation myocardial infarction, an indication for dobutamine, or those in the beta-blocker up-titration phase were excluded. This trial demonstrated no difference in clinical improvement (defined as improvements in dyspnea or general well-being on a 5-point scale) at both 3 and 8 days, suggesting that continuation of beta-blocker therapy did not worsen outcomes. Patients in the continuation group were also more likely to be on beta-blocker therapy at 3 months, confirming that continuation of beta-blocker therapy in ADHF also helps with optimization of GDMT post-discharge.
A more recent meta-analysis evaluated outcomes associated with beta-blocker discontinuation in ADHF and found that beta-blocker withdrawal significantly increased the risk of in-hospital mortality (RR: 3.72; 95% CI: 1.51 to 9.14).7In addition, mortality between 60 and 180 days was increased in patients not continued on a beta-blocker (RR: 1.78; 95% CI: 1.13 to 2.79), as was the combined endpoint of mortality between 60 and 180 days and rehospitalization (RR: 1.84; 95% CI: 1.08 to 3.1). Such findings are consistent with other studies showing worse post-discharge outcomes when beta-blocker therapy is inappropriately discontinued.8The importance of ensuring appropriate GDMT in HF patients prior to discharge will be further discussed in an upcoming blog (stay tuned!).
In patients admitted with ADHF, defining an underlying etiology is important for determining the proper management of beta-blocker therapy (see below for a list of other potential etiologies).9In those who have been on a stable dose of beta-blocker without recent initiation or up-titration, beta-blocker therapy is not likely the cause of the exacerbation. As such, beta-blockers should be continued in these patients. Importantly, doses should not be increasedduring ADHF (even if the patient is presenting with atrial fibrillation requiring rate control) and should only be considered once a patient is euvolemic.
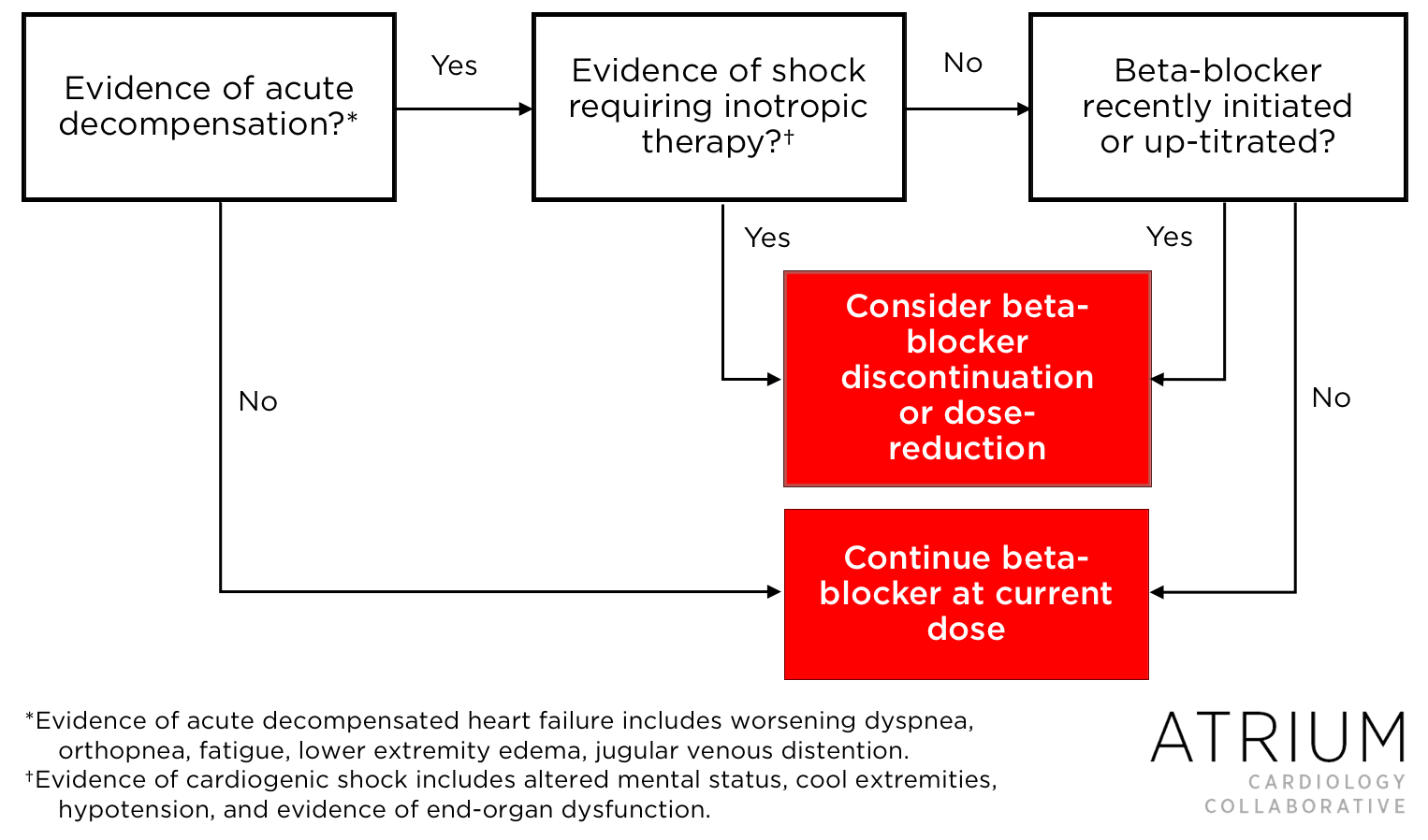
Despite the benefits of continued therapy, there are certain situations in which beta-blocker therapy should be dose-reduced or discontinued altogether, and we’ve created a tool to assist in this decision-making (Figure 1). It should especially be considered in patients who are hemodynamically unstable or in those with suspected cardiogenic shock.
A small subset of patients with advanced heart failure may require continued administration of inotropic therapy even after ADHF has resolved, and the use of beta blockers in this setting remains controversial. Interestingly, some evidence supports concurrent use of beta blockers and inotropes in patients receiving inotropes as a bridge to more definitive therapies (e.g., a ventricular assist device or cardiac transplantation) or for symptom palliation.10Although there are often concerns that beta-blockers will counteract the effects of inotropic therapy, studies have shown that this is not always the case, particularly with regard to milrinone.11Thus, in patients on stable regimens who require inotropic therapy, continuation of beta-blockade could be of benefit, including the mitigation of arrhythmias associated with these agents. However, decisions about beta-blocker therapy in this setting should weigh patient-specific risks and benefits.
In summary, although continuing beta-blockers in the setting of ADHF seems counterintuitive, every effort should be made to do so in the absence of shock or hemodynamic instability. Continuing beta-blockers in this setting has been shown to improve both in-hospital and post-discharge outcomes. Beta-blocker discontinuation and/or dose reduction should only be considered in those patients with ADHF presenting with shock syndromes requiring inotropic therapy and/or those with recent beta-blocker initiation/up-titration preceding decompensation.
 |
Stormi Gale, PharmD, BCPS
|
References:
- Hjemdahl P, Olsson G. Rebound phenomena following withdrawal of long-term beta-adrenoceptor blockade. Acta Med Scand Suppl. 1982;665:43–7.
- O’Brien ET. Beta-blockade withdrawal. Lancet. 1975 Oct 25;2(7939):819.
- Modany A, Walter C, Clarke M, Klootwyk J, Stollar K, Sokos GG. Ability to Achieve Target Doses of an Evidence-based Heart Failure Treatment Regimen in an Advanced Heart Failure Clinic at a Tertiary Care Facility. Journal of Cardiac Failure. 2015 Aug 1;21(8):S52.
- Bristow MR, Gilbert EM, Abraham WT, Adams KF, Fowler MB, Hershberger RE, et al. Carvedilol produces dose-related improvements in left ventricular function and survival in subjects with chronic heart failure. MOCHA Investigators. Circulation. 1996 Dec 1;94(11):2807–16.
- Fiuzat M, Wojdyla D, Kitzman D, Fleg J, Keteyian SJ, Kraus WE, et al. Relationship of -Blocker Dose with Outcomes in Ambulatory Heart Failure Patients with Systolic Dysfunction: Results from the HF-ACTION Trial. J Am Coll Cardiol. 2012 Jul 17;60(3):208–15.
- Jondeau G, Neuder Y, Eicher J-C, Jourdain P, Fauveau E, Galinier M, et al. B-CONVINCED: Beta-blocker CONtinuation Vs. INterruption in patients with Congestive heart failure hospitalizED for a decompensation episode. Eur Heart J. 2009 Sep 1;30(18):2186–92.
- Prins KW, Neill JM, Tyler JO, Eckman PM, Duval S. Effects of Beta-Blocker Withdrawal in Acute Decompensated Heart Failure: A Systematic Review and Meta-Analysis. JACC: Heart Failure. 2015 Aug 1;3(8):647–53.
- Fonarow GC, Abraham WT, Albert NM, Stough WG, Gheorghiade M, Greenberg BH, et al. Influence of beta-blocker continuation or withdrawal on outcomes in patients hospitalized with heart failure: findings from the OPTIMIZE-HF program. J Am Coll Cardiol. 2008 Jul 15;52(3):190–9.
- Joseph SM, Cedars AM, Ewald GA, Geltman EM, Mann DL. Acute Decompensated Heart Failure. Tex Heart Inst J. 2009;36(6):510–20.
- Shakar SF, Abraham WT, Gilbert EM, Robertson AD, Lowes BD, Zisman LS, et al. Combined oral positive inotropic and beta-blocker therapy for treatment of refractory class IV heart failure. J Am Coll Cardiol. 1998 May;31(6):1336–40.
- Metra M, Nodari S, D’Aloia A, Muneretto C, Robertson AD, Bristow MR, et al. Beta-blocker therapy influences the hemodynamic response to inotropic agents in patients with heart failure. Journal of the American College of Cardiology. 2002 Oct;40(7):1248–58.
Share this post:

Pingback: LITFL Review 343 • LITFL