Share this post:
Author: Zachary R. Noel, PharmD, BCCP
Patients with non-valvular atrial fibrillation (NVAF) undergoing percutaneous coronary intervention (PCI) for coronary artery disease (CAD) often have an indication for both anticoagulation (ie, vitamin K antagonist or direct oral anticoagulant) as well as dual antiplatelet therapy (DAPT) with aspirin and a P2Y12 inhibitor. This is colloquially referred to as “triple therapy”, meaning three unique antithrombotic drugs, each with a different mechanism of action, are being used to prevent thromboembolic events related to NVAF and CAD. In patients with NVAF, cardioembolic stroke is predominately due to hemostasis and thrombus formation within the left atrium. Anticoagulants are effective at preventing this, whereas, in comparison, antiplatelet drugs are largely ineffective .1-3 On the contrary, intra-coronary stent-related complications are predominately platelet-mediated; hence, antiplatelet medications are the backbone for prevention of stent thrombosis as well as for prevention recurrent myocardial infarction.4 While preventing thromboembolic complications is critical, it must be balanced against the increased risk of severe bleeding complications associated with this practice. Furthermore, if triple therapy is used it remains unclear what the optimal duration should be before transitioning to dual therapy (ie, oral anticoagulant and a P2Y12 inhibitor).
Recently, a series of trials evaluated the safety of dual antithrombotic therapy (oral anticoagulant and a P2Y12 inhibitor) compared to standard triple therapy in patients with AF and recent PCI and/or an acute coronary syndrome (ACS) (Table 1).5-7 In the PIONEER-AF, RE-DUAL PCI, and AUGUSTUS trials, dual therapy with a direct oral anticoagulant (DOAC) and P2Y12 inhibitor (namely clopidogrel) demonstrated significantly less bleeding with similar rates of thromboembolic events compared to triple therapy. The totality of the evidence strongly suggests “less is more” and that withholding aspirin markedly reduces major bleeding events without warning signals that it compromises efficacy (of note, these trials were not powered to detect differences in thromboembolic endpoints). While many practitioners have been quick to adopt dual antithrombotic therapy (myself included), it is important to consider the external validity of these trials and how we apply them to our patients before throwing in the towel on triple therapy.
Consideration #1: Timing of Aspirin Discontinuation in Clinical Trials
In the aforementioned landmark clinical trials, the time to enrollment following PCI was quite variable (Table 1). In AUGUSTUS, for example, the average time to enrollment was 6 days but could be as far out as 14 days. During the interim period following PCI and before enrollment, patients were treated with standard of care (ie, triple therapy). While this may seem insignificant, it is well established that the risk of stent thrombosis is greatest in the early period (ie, 24 hours – 30 days) following stent placement.8-9 Although the risk for stent thrombosis with modern PCI techniques is quite low (ie, <1%), the risk still remains greatest in the immediate hours-days following stent placement, hence there may be added benefit in continuing aspirin during this vulnerable period (ie, until hospital discharge, if applicable). This may be particularly true for patients on warfarin with a subtherapeutic INR who are not receiving parenteral anticoagulation.
| Table 1. Landmark Clinical Trials Comparing Dual vs Triple Antithrombotic Therapy in Patients with NVAF Undergoing PCI | |
| Trial (year) | Time from Index Event to Enrollment* |
| PIONEER-AF (2016)
Open-Label, Randomized, Controlled, Multicenter Study Exploring Two Treatment Strategies of Rivaroxaban and a Dose-Adjusted Oral Vitamin K Antagonist Treatment Strategy in Subjects with Atrial Fibrillation who Undergo Percutaneous Coronary Intervention |
72 hours, but could receive aspirin for 24 hours after enrollment |
| RE-DUAL PCI (2017)
Randomized Evaluation of Dual Antithrombotic Therapy with Dabigatran versus Triple Therapy with Warfarin in Patients with Nonvalvular Atrial Fibrillation Undergoing Percutaneous Coronary Intervention |
Within 120 hours |
| AUGUSTUS (2019)
An Open-label, 2 x 2 Factorial, Randomized Controlled, Clinical Trial to Evaluate the Safety of Apixaban vs. Vitamin K Antagonist and Aspirin vs. Aspirin Placebo in Patients with Atrial Fibrillation and Acute Coronary Syndrome or Percutaneous Coronary Intervention |
3 – 14 days (median 6.7 days) |
*In AUGUSTUS, the index event was either acute coronary syndrome (with or without PCI) or elective PCI. In RE-DUAL PCI and PIONEER AF the index event was acute coronary syndrome requiring PCI, or elective PCI
Consideration #2: Patients Not Represented in Clinical Trials
There were many similarities across the three trials highlighted in Table 1. For example, the average age was ~70 years old in each trial, 50-60% presented with an acute coronary syndrome, and the average CHA2DS2-VASc was ~4. Furthermore, each trial excluded certain patient populations that directly affect the external validity of the results. Table 2 includes patient populations and comorbidities not represented, or underrepresented, where triple therapy may be justified on a case-by-case basis.
| Table 2. Underrepresented Populations in Landmark Clinical Trials of Atrial Fibrillation and PCI |
| Known thrombophilia, history of venous thromboembolism, or active malignancy |
| Valvular atrial fibrillation (ie, mechanical valve or mitral stenosis)† |
| Peripheral vascular disease |
| Age less than 50-60 years |
| Chronic kidney disease (ie, creatinine clearance < 30-60 ml/min.) |
| *History of ischemic stroke |
| **High-risk features for stent-driven recurrent ischemic events |
†Warfarin remains the anticoagulant of choice in valvular atrial fibrillation
*Patients with a history of stroke were excluded from PIONEER-AF, and only ~10-15% of patients had a history of stroke in RE-DUAL PCI and AUGUSTUS.
**Examples include prior stent thrombosis, diffuse multivessel disease in patients with diabetes, bifurcating stents, treatment of chronic total occlusions, and total stent length > 60 mm, among other factors10
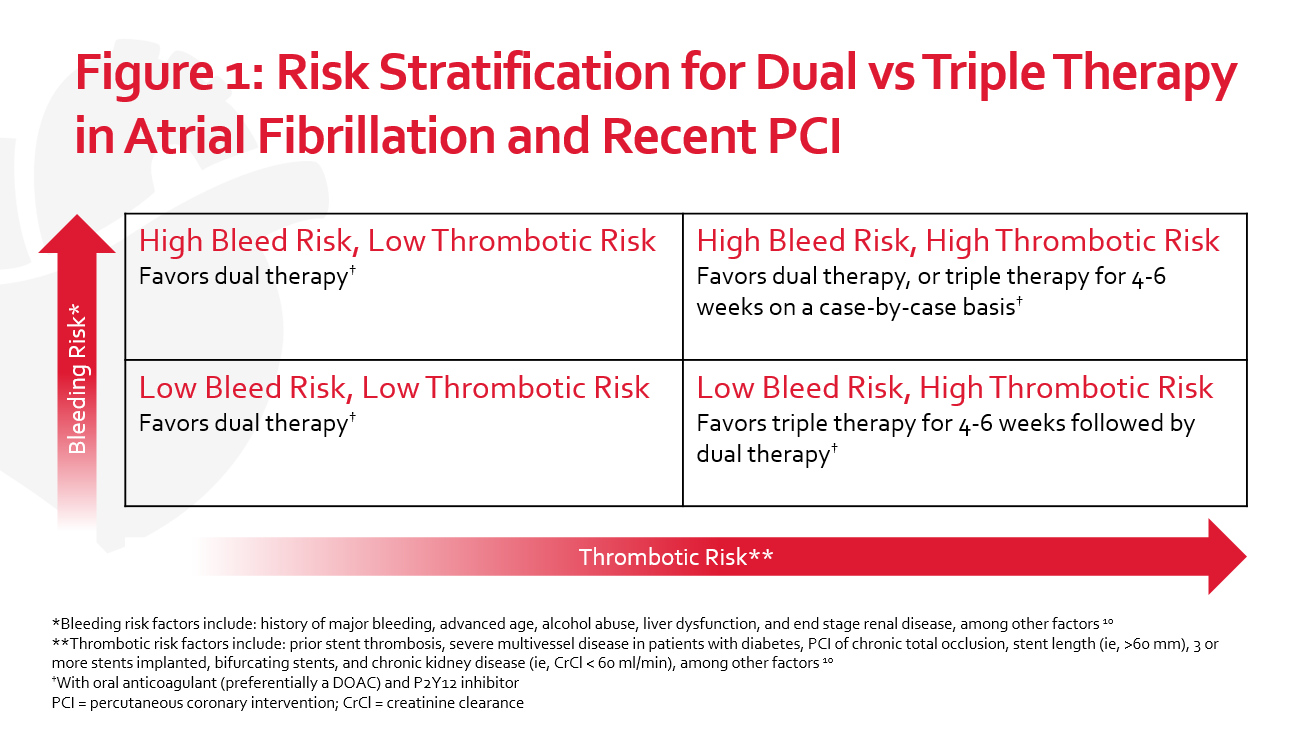
At our institution, we have adopted dual therapy for most patients, but not all. Figure 1 provides guidance on how to ascertain when triple therapy may be warranted. As a case example, we recently used triple therapy in a patient presenting with an acute coronary syndrome who had severe multivessel disease requiring high-risk, staged PCI. In addition, the patient had peripheral vascular disease, diabetes, and Factor V Leiden. Aside from the patient’s age, there were no apparent risk factors for bleeding. As such, the patient was considered “low bleed risk, high thrombotic risk”. The patient was ultimately discharged home with warfarin, clopidogrel, and aspirin with instructions to discontinue aspirin after 4 weeks. Warfarin was chosen given the patient’s history of Factor V Leiden, in addition to the patient being on two strong CYP 3A4 inducers which made using a DOAC contraindicated. A duration of 4 weeks was chosen in an attempt to balance the risk of thrombotic events with the bleeding risk associated with longer durations of triple therapy. It’s important to note that decisions on an appropriate antithrombotic regimen should be multidisciplinary and include the interventional cardiologist, pharmacist, and, most importantly, the patient.
Consideration #3: Clopidogrel Genotyping and Alternative P2Y12 Inhibitors
Approximately 90-95% of patients in PIONEER-AF, RE-DUAL PCI, and AUGUSTUS received clopidogrel, and the remainder ticagrelor. Interestingly, none of these trials routinely performed or reported CYP 2C19 genotyping results. In theory, poor or intermediate metabolizers receiving dual therapy with clopidogrel are at a heightened risk of thromboembolic events compared to normal metabolizers. Furthermore, using triple therapy in poor or intermediate metabolizers may offset the added thromboembolic risk. Another way to mitigate this risk is to empirically switch to ticagrelor, though some remain hesitant to do so, citing concerns for bleeding. Ultimately, additional studies are needed to elucidate how to proceed in this setting.
Conclusion
Guideline recommendations for the use of triple versus dual therapy in patients with atrial fibrillation and recent percutaneous coronary intervention have not been updated since the release of PIONEER-AF, RE-DUAL PCI, and AUGUSTUS.11 The use of dual therapy (preferably with a DOAC and P2Y12 inhibitor) has consistently shown a reduction in bleeding events compared to triple therapy and is an attractive option for patients at heightened risk of bleeding and/or low thromboembolic risk. Nonetheless, important limitations have been highlighted in this blog that warrant consideration prior to throwing in the towel on triple therapy.
 |
Zachary R. Noel, PharmD, BCCP
|
References
- The ACTIVE Investigators. Effect of clopidogrel added to aspirin in patients with atrial fibrillation. N Engl J Med 2009; 360:2066-78.
- Connolly S, Pogue J, Hart R, et al. Clopidogrel plus aspirin versus oral anticoagulation for atrial fibrillation in the Atrial fibrillation Clopidogrel Trial with Irbesartan for prevention of Vascular Events (ACTIVE W): a randomised controlled trial. Lancet 2006;367:1903-12.
- Connolly S, Eikelboom J, Campbell J, et al. Apixaban Versus Acetylsalicylic Acid [ASA] to Prevent Stroke in Atrial Fibrillation Patients Who Have Failed or Are Unsuitable for Vitamin K Antagonist Treatment. N Engl J Med 2011; 364:806-17.
- Mehta S, Salim Y, Peters R, et al. Effects of pretreatment with clopidogrel and aspirin followed by long-term therapy in patients undergoing percutaneous coronary intervention: the PCI-CURE study. Lancet 2001;358: 527-33.
- Gibson CM, Mehran R, Bode C, et al. Prevention of bleeding in patients with atrial fibrillation undergoing PCI. N Engl J Med 2016; 375: 2423-34.
- Cannon CP, Bhatt DL, Oldgren J, et al. Dual antithrombotic therapy with dabigatran after PCI in atrial fibrillation. N Engl J Med 2017; 377: 1513-24.
- Lopes RD, Heizer G, Aronson R, et al. Antithrombotic Therapy after Acute Coronary Syndrome or PCI in Atrial Fibrillation. N Engl J Med 2019;380(16):1509-1524.
- Van Werkum JW, Heestermans AA, Zomer AC, et al. Predictors of Coronary Stent Thrombosis: The Dutch Stent Thrombosis Registry. J Am Coll Cardiol. 2009;53:1399-1409.
- Holmes DR Jr, Kereiakes DJ, Garg S, et al. Stent thrombosis. J Am Coll Cardiol. 2010;56:1357-65.
- Valgimigli M, Bueno H, Byrne RA, et al. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS. European Journal Of Cardio-Thoracic Surgery: Official Journal Of The European Association For Cardio-Thoracic Surgery. 2018;53(1):34-78.
- Levine GN, Bates ER, Bittl JA. 2016 ACC/AHA Guideline Focused Update on Duration of Dual Antiplatelet Therapy in Patients With Coronary Artery Disease. J Am Coll Cardiol. Sep 2016, 68 (10) 1082-1115.
Share this post: